What is glaucoma?
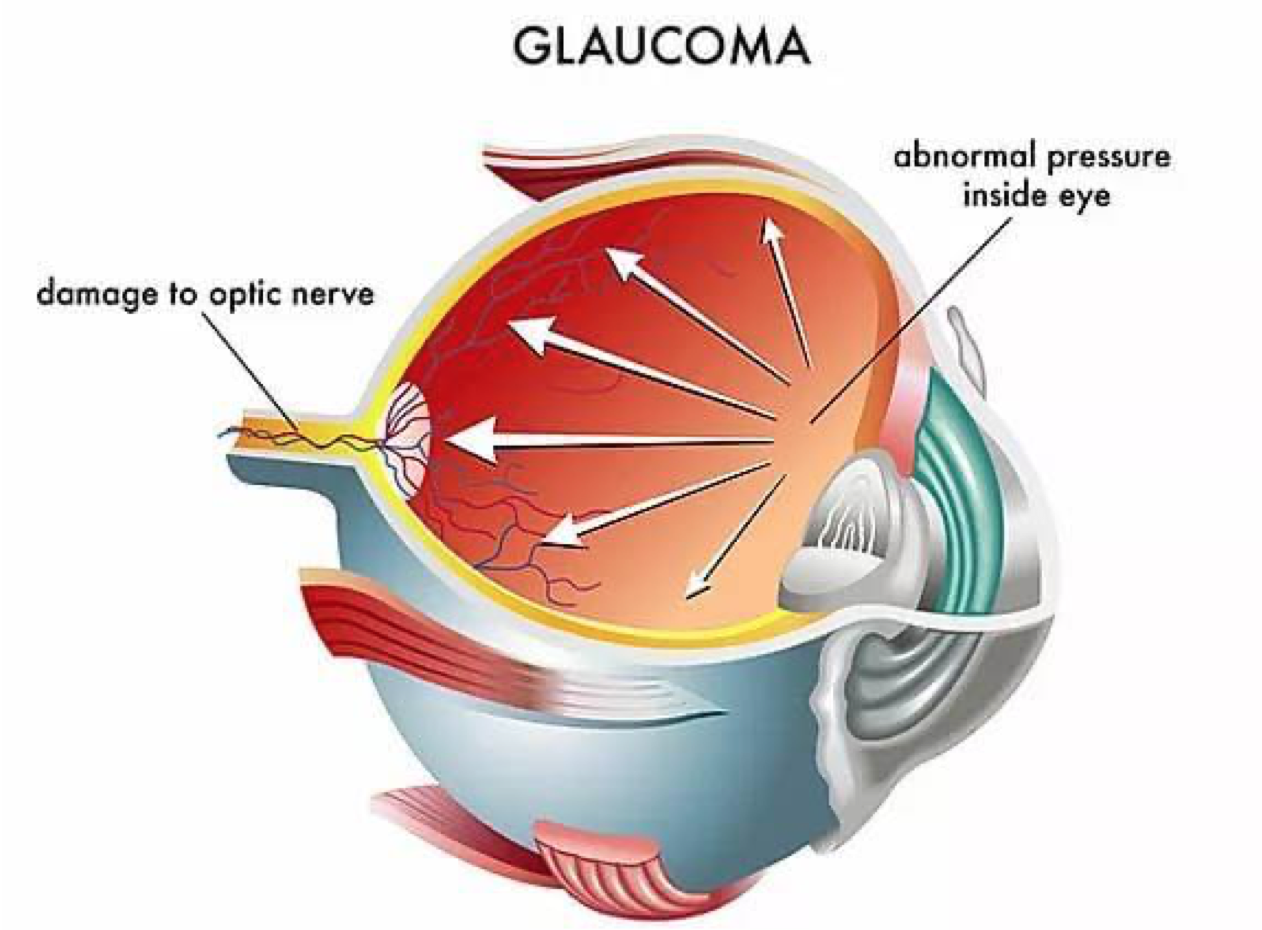
Glaucoma is a disease that damages your eye’s optic nerve. It usually happens when the fluid (called aqueous humour) builds up in the front part of your eye. That extra fluid increases the pressure in your eye, damaging the optic nerve.
Glaucoma is a leading cause of blindness for people over 60 years old. But blindness from glaucoma can often be prevented with early treatment.
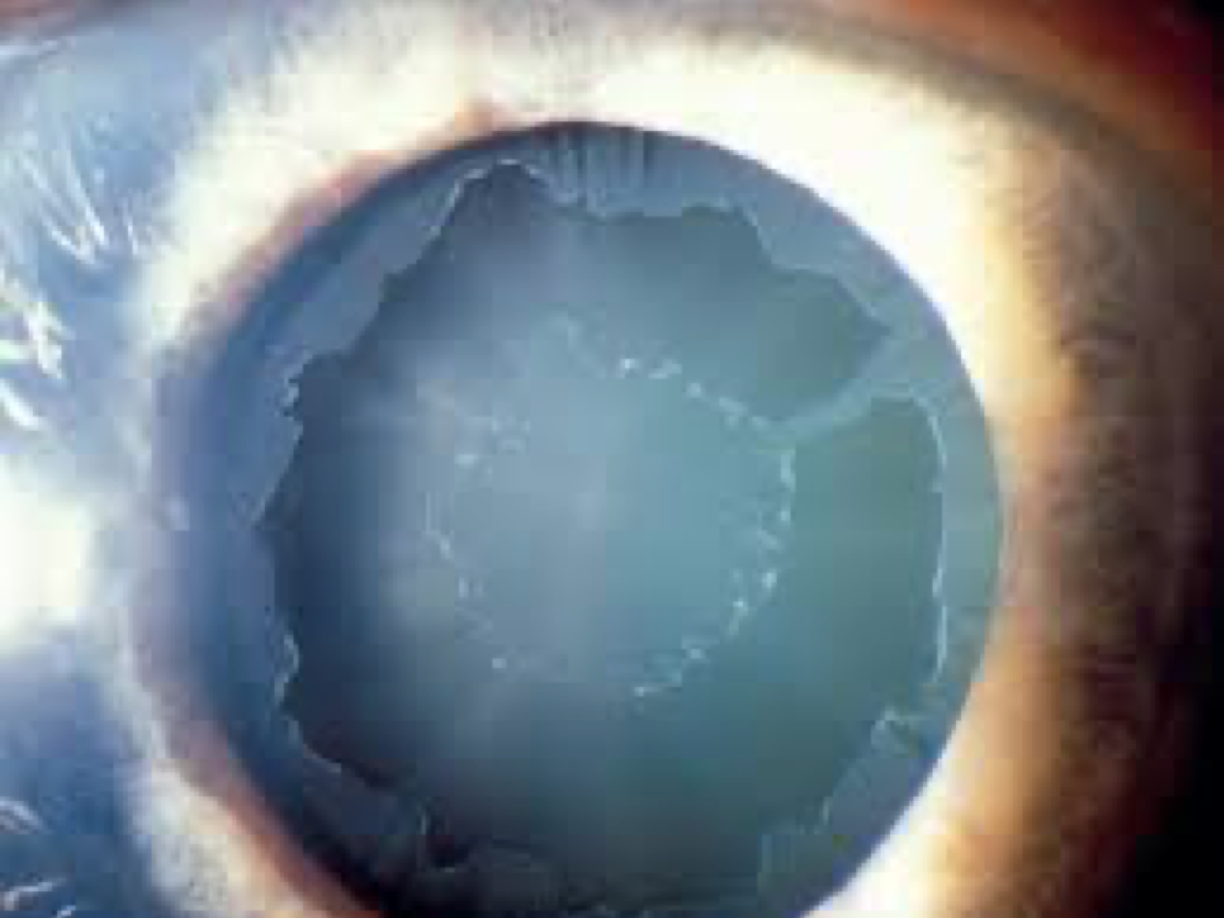
Pseudoexfoliation syndrome (or PXF, also sometimes called Exfoliation Syndrome) is when tiny flakes of dandruff-like material build up in the body.
These microscopic clumps of protein fibers are produced throughout the body, including the lung, skin, liver, heart, kidney, and gallbladder, just to name a few. However, it only manifests as a disease in the eye, where there are flakes of material at the edge of the pupil, on the lens, in the drainage structures, and throughout other structures primarily in the front of the eye. When the eye’s drainage system is clogged by this flaky pseudoexfoliative material, as well as pigment, the eye pressure can increase and lead to glaucoma and loss of vision.
Pseudoexfoliation glaucoma, or pseudoexfoliative glaucoma, is the same condition with the addition of elevated eye pressure and evidence of damage to the optic nerve.
Pseudoexfoliation is not to be confused with “true exfoliation”, which is due to heat or infrared exposure (and which can be found among glassblowers).
Doctors do not know for sure why people get PXF. Most think there are both genetic (passes down in families) and environmental causes (caused by something in the envirionmenet. PXF is rare in people younger than 50. This points to age-related changes in the tissues of the eye, which is true of many eye diseases. confused with “true exfoliation”, which is due to heat or infrared exposure (and which can be found among glassblowers).
It is rarely seen before the age of 50, and its incidence increases with age. It is more common in women than in men. There is a high prevalence of pseudoexfoliation syndrome in Scandinavian countries, where it is estimated that 50 percent of open-angle glaucoma is caused by pseudoexfoliation syndrome. On the other hand, it is relatively rare among African Americans and Eskimos. However, it is also seen more often in Europe, the Middle East, South Africa, and South America. Indeed, pseudoexfoliation syndrome is likely found in all populations. In addition to age, gender, and race, another risk factor is genetics. Some people carry a variant in the LOXL1 gene that is a risk factor for pseudoexfoliation glaucoma.
PXF glaucoma does not have any noticeable symptoms. High pressure inside the eye does not cause any pain, so patients can slowly lose vision without knowing it.
An ophthalmologist can usually find signs of PXF during a comprehensive eye exam. Tests they may do include:
A slit lamp. Your ophthalmologist uses the bright light and microscope of the slit lamp to look.
Although there are patients in whom pseudoexfoliation material is seen but there is no sign of glaucoma, it is estimated that approximately 40 – 50 percent of patients who have pseudoexfoliation syndrome will eventually develop glaucoma. Therefore, it is important for those who are diagnosed with this syndrome (which is symptomless and therefore requires an ophthalmic examination to diagnose), to be followed over time in order to monitor for the development of glaucoma. Indeed, sometimes pseudoexfoliation syndrome is subtle and can be missed. A careful examination by an ophthalmologist, including a detailed look for tiny flakes of PXF material at the front of the eye (on the iris and lens) and drainage angle, and also a dilated eye exam, will help to determine the diagnosis.
Unfortunately, eye pressure can be quite high in this disease, and can be more difficult to control than in primary open-angle glaucoma. It is often associated with worse field of vision loss and greater optic nerve damage than in patients who have primary open-angle glaucoma. Indeed, sometimes pseudoexfoliation glaucoma can even be associated with angle-closure glaucoma because the material deposits on portions of the eye that keep the lens in the correct position. When these structures become weak, the lens can come forward and cause the angle to narrow.
In addition, as with all glaucomas, the treatment for pseudoexfoliation glaucoma is to lower the eye pressure. Unfortunately, sometimes medications will fail to control the eye pressure, although laser can be very effective. Finally, surgeries such as trabeculectomy are sometimes needed for long-term eye pressure control.
Pseudoexfoliation syndrome and pseudoexfoliation glaucoma also present unique challenges when considering cataract surgery. Just as described above, when material deposits on the structures holding the lens in place, these structures are weaker and will predispose the patient to increased risk of complications during cataract surgery, or even late dislocation of the implanted intraocular lens over time. However, the surgeon will take extra precautions to avoid these complications. In addition, it is sometimes recommended that patients not wait too long before cataract surgery because the surgery becomes more difficult if the cataract is very dense or mature. If you have pseudoexfoliation syndrome or pseudoexfoliation glaucoma it is important to have a frank discussion with your ophthalmologist prior to cataract surgery so that you fully understand the risks.
Is there anything one can do to prevent pseudoexfoliation syndrome? Much research is ongoing to try to understand the environmental risk factors that predispose one to developing pseudoexfoliation in the first place. At this point, however, the best recommendations are the same as for all age-related eye diseases: get a comprehensive eye examination by an eye doctor (baseline at age 40, and every 1-2 years for seniors age 65 and over) and wear sunglasses. If you are diagnosed with pseudexfoliation syndrome, it is important to maintain follow-up visits with your ophthalmologist to monitor for the development of glaucoma.
Pseudoexfoliation does not have any symptoms. This is why it’s important to see your ophthalmologist regularly. If glaucoma is found early enough you can save your vision.
